 In the organ transplantation field, the ELISPOT assay is used as a reliable tool as guide for therapeutic interventions after transplantation. Different studies have shown that the number of IFN-γ producing T cells correlate with post transplantation outcome. For example, an increased frequency of donor-specific IFN-γ producing cells before transplantation was related to the risk of acute rejection and impaired post transplant function.
In the organ transplantation field, the ELISPOT assay is used as a reliable tool as guide for therapeutic interventions after transplantation. Different studies have shown that the number of IFN-γ producing T cells correlate with post transplantation outcome. For example, an increased frequency of donor-specific IFN-γ producing cells before transplantation was related to the risk of acute rejection and impaired post transplant function.
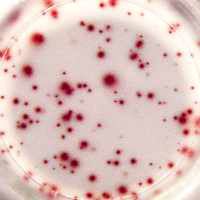
Some studies have suggested the involvement of IL-17 in human allograft rejection. Naïve human CD4 T cells can differentiate into Th17 cells, secreting the pro-inflammatory cytokines IL-17A and IL-22. Th17 cells express CCR4, CCR6 and STAT4 and are clearly pathogenic, thereby challenging the importance of classical Th1 cells in the induction and maintenance of chronic inflammatory disease. As a result of these properties, the IL-17 family has been linked to various immune/autoimmune related diseases including rheumatoid arthritis, asthma, lupus, anti-tumor immunity, and also allograft rejection. Recently, Van Besouw et al. (2015) measured the frequency of IL-17A producing cells reactive to donor cells in peripheral blood mononuclear cells (PBMC) of heart transplant patients with U-Cytech’s IL-17A ELISPOT assay (CT416). The authors demonstrated circulating donor-reactive IL-17A producing cells only during immunologic quiescence (without acute rejection [AR]), and not in PBMCs collected from heart transplant recipients with early (≤ 3 months) or late (> 3 months) AR.